Our Health
Welcome to the WQPHN 2021-2022 Annual Report Highlights. For a printable version of the report, please click here.
Responding to COVID-19
COVID Communications
Throughout the year communications played a vital role in keeping communities, staff and health professionals up to date with the latest news, data reports and changes to COVID health advice.
WQPHN continued to inform our communities on a regular basis across a range of communication platforms including Facebook, newsletters, emails, website updates and publications.
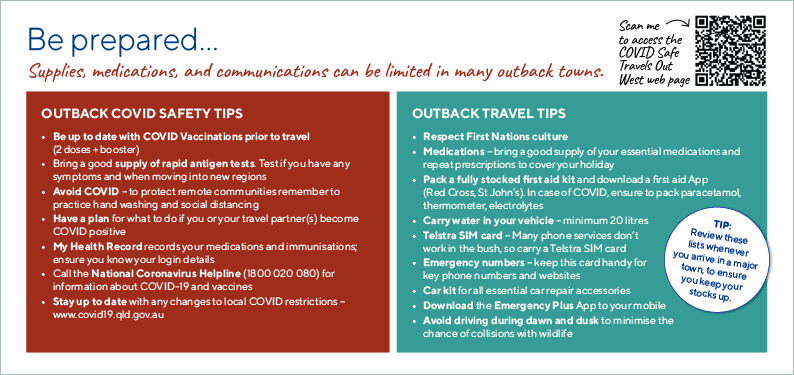
Targeted campaigns were aimed at reducing the spread of COVID-19 across our vulnerable communities, including the COVID SAFE TRAVELS OUT WEST Campaign. The campaign included postcards and posters distributed across Western Queensland with key health messages and travelling tips targeting the "Grey nomads", linking directly to a dedicated COVID Safe Travels page on the WQPHN Website.

Vaccination
WQPHN continued the successful roll-out of targeted vaccination clinics (pop-ups) across the region in 2021-22. A strong focus was on hard-to-reach populations, particularly First Nations peoples and remote communities with limited access to vaccinations.
Working in close collaboration with our health partners WQPHN coordinated schedules, vaccination locations and administration sites, and utilised the services of vaccination teams, directly funded by the Department of Health.
Community Care Pathways
The COVID-19 Response team worked with Queensland Health clinical leads, Healthdirect, our ACCHS, GP’s and other stakeholders to develop and update community care pathways. These pathways provided clear plans for where and how patients were managed in the primary and community care system, depending on their clinical risk and severity of illness. Pathways also identified escalation arrangements for people who needed to be admitted to a virtual ward (hospital in the home) for more intense observation or admitted to hospital.
PPE
As our Health Services continued the challenge of managing COVID-positive patients, WQPHN was able to support General Practices, ACCHSs, and Community Pharmacies across Western Queensland by supplying and distributing Personal Protective Equipment (PPE) to allow practitioners to safely continue their vital work. During this period WQPHN distributed more than:
30000Surgical Masks9500P2/N95 respirators5500Pairs of Gloves3000Isolation Gowns700Face Shields500Protective Goggles200Pulse Oximeters100Bottles of Hand Santiser


Our Stories
Western Queensland Aged Care leads the way in COVID prevention
The steady achievers in 2021/22 have once again been the committed staff working in residential and community aged care. Throughout the added stress of COVID-19, they persevered through the hugely increased information flow from the sector, supporting their elderly frail residents with multiple vaccinations and the many lock downs that were so difficult for all involved.
In the words of Betty Kiernan, Director, Laura Johnson Home, “we’re still walking, we’re still on this journey” reflecting on her experience keeping the residents in Mount Isa safe.
Videos
Learn more about the COVID-19 experience from Betty Kiernan.
COVID-19 Campaign - Booster Shots
Strategy 1: Integrating Care
Supporting collaboration with primary health care partners and lead co-design to enable integrated service frameworks on key health priorities.Working together with our partner organisations has continued to strengthen in 2021-22 assisting a coordinated approach towards the shared goal of better health for Western Queenslanders.
Nukal Murra Alliance

Nukal Murra Alliance (NMA) members work collaboratively with other funded agencies to support the re-direction of funds to Indigenous Health programs through the Nukal Murra Health Support Services to improve the health, social and emotional wellbeing of our communities across the Western Queensland region.
Key members of the Alliance met in October to discuss significant Strategic Health Reports for planning and review over the next 3-5 years for Indigenous Health in the Western Queensland Region.
Initiatives will include but not be limited to over the next 12 months:
- Grow Your Own Workforce Program – Developed to build the capacity of the health workforce, particularly regional, rural and remote areas by supporting place-based education to employment opportunities within NMA organisations.
- Virtual Health Services (VHS) Program - Goondir Aboriginal Medical Services was chosen to manage and administer the VHS Program across the Alliance Organisations. The implementation of the program aims to improve the health and well-being of Aboriginal and Torres Strait Islander people to a standard level equal to the wider Australian community.
Nukal Murra Alliance organisations will be equipped with the appropriate medical resources and devices to deliver programs in a culturally appropriate and sensitive manner..
- Social and Emotional Wellbeing - SEWB – WQPHN has recruited a full-time SEWB Regional Coordinator as a 12 month funding project to undertake and build capacity of NMA services, to enhance existing mental health services and mental health promotional supports for our First Nation people. Training and development strategies will include addressing a skill shortage in the areas of recruitment and retention of SEWB Champions and Trainers.
- SEWB and Mental Health Training and Development Program - developed to support all NMA Organisations. The Program has been rolled out and provided to two of the member services by an Outreach Private Consultant Service “Wakai Waian Healing” and Founder, Mr Edward Mosby (Senior Psychologist). The Service provides support with delivery of individual and group therapeutic services, supports local SEWB Workers and their co-workers with mentoring/supervision with the view towards professional development and self-care as well as providing direct support and guidance towards enhancement of community and service collaboration and capacity building efforts.
- Alliance ITC Program - The Care Access Manager commissioned through CWAATSICH has commenced scheduling dates for community and stakeholder visits, including care coordination services of clients across the WQ region.
Nukal Murra Report Cards continue to be supplied regularly to NMA and Clinical Chapter members to measure the uptake of ITC services.
Reshaping the way we deliver health services through the Nukal Murra Health Support Service also has considerable impact on the public health system - saving $3.48 in avoided hospital costs for every $1 invested.Maranoa Accord
Partners in the Maranoa Accord: WQPHN, NWHHS, CWHHS, SWHHS, CACH, CWAATSICH, Goondir Health Services and Gidgee Healing continue to work together and lead whole of population improvements in Western Queensland.
Through the Western Queensland Health Services Integration Committee (WQHSIC), the partner organisations:
- continued to monitor the collective efforts in relation to the COVID-19 vaccination rollout in 2021-22;
- shared outcomes from local needs assessments conducted in 2021-22; and
- collaborated on the development of Health Equity Strategies.
The CEOs of The Maranoa Health Accord plan to work further on the shared key priorities from the health strategy plans to inform a local Primary Health Care Strategy for Western Queensland.
North West Tripartite Agreement
For the North West Tripartite Agreement partners;
- Gidgee Healing
- North West Hospital and Health Service and
- WQPHN
With COVID-19 making it difficult for the leaders of partner organisations to meet face-to-face, we continued to work together through on-the-ground services in our commitment to improve the health of the Aboriginal and Torres Strait Islander people of North West Queensland. The CEOs and Chairs of the partner organisations plan to work further on strengthening the Tripartite Agreement in the coming year.
Strategy 2: WQ Health Care Home (WQ HCH)
Strengthening general practice and service provider capability and innovation building a contemporary patient centred primary health care strategy.WQ Health Care Home
The Western Queensland Health Care Home (WQ HCH) program is a suite of self-evaluation, education, training, data analysis, and quality improvement tools and resources to help primary care practices operate efficiently and effectively.
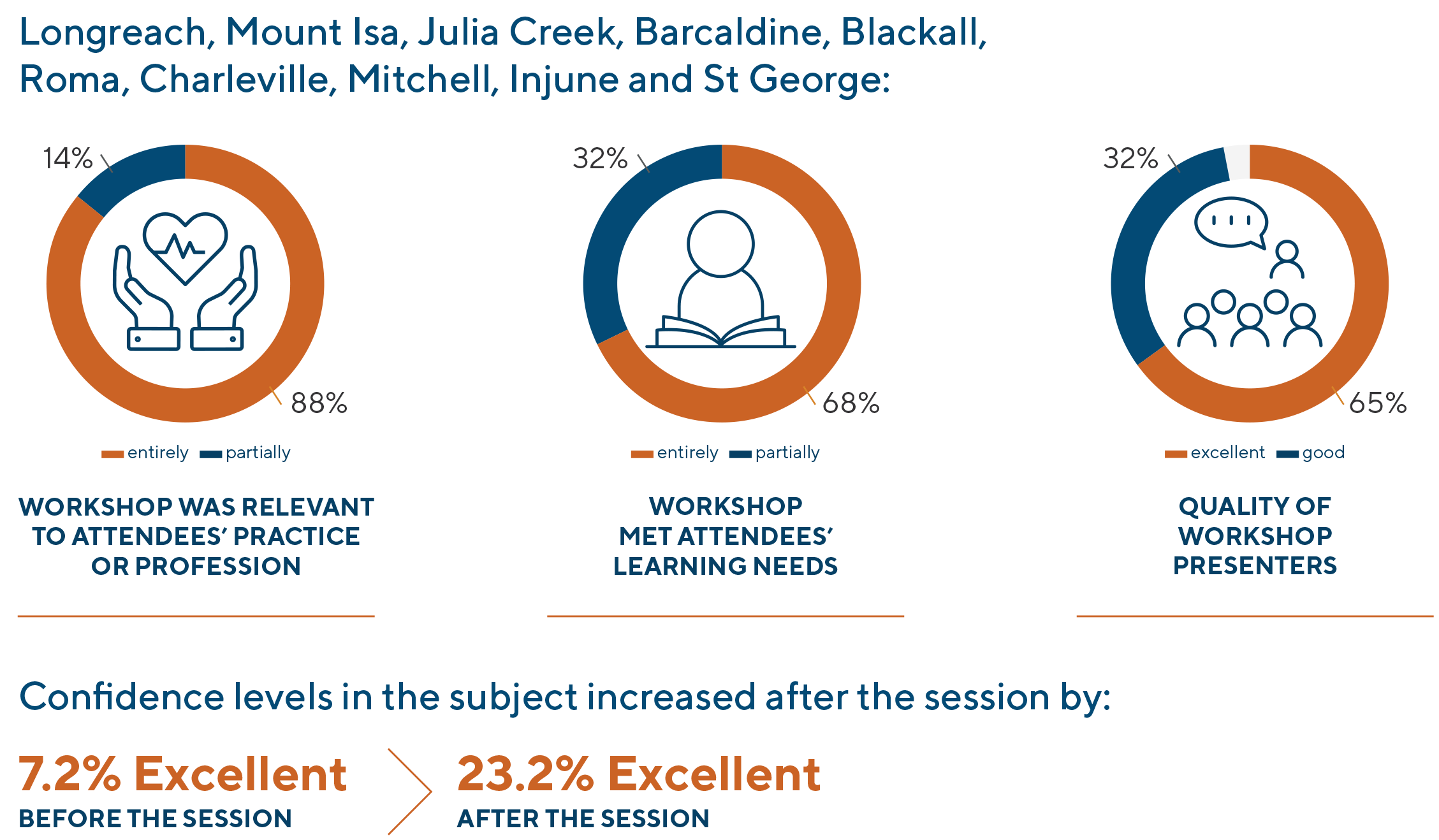
Workshops are held each year and the 2021-22 year’s workshops focused on investigating the demographics of local communities, and how to integrate and utilise other local health and community services. The workshops blended theory, data, interactive, and practical components, and provided protected planning time for practices away from the busy day-to-day operations. Understanding practice data and populations provided a platform to look at ways to improve Chronic Disease management using the roles of Care Coordination and Team Based Care. The added benefit of the workshops was the ability for practice staff to network and meet likeminded people within their region.
Over 2021-22 the Practice Capability and Innovation Team delivered 12 Quality Improvement workshops to 18 Western Queensland Health Care Homes practices. The team visited 11 General Practices across the North West, Central West, and South West regions collaborating with 119 attendees.


Responses to attendance satisfaction surveys were positive, with 97% of participants indicating the learning objectives were met by the sessions.
Key to the success of the WQ HCH program is the ability of practices to utilise the tools and resources provided by WQPHN to drive continual quality improvement initiatives. As each year progresses, the practices have learnt and grown and implemented the skills and tools of the WQ HCH program into their Quality Improvement activities.
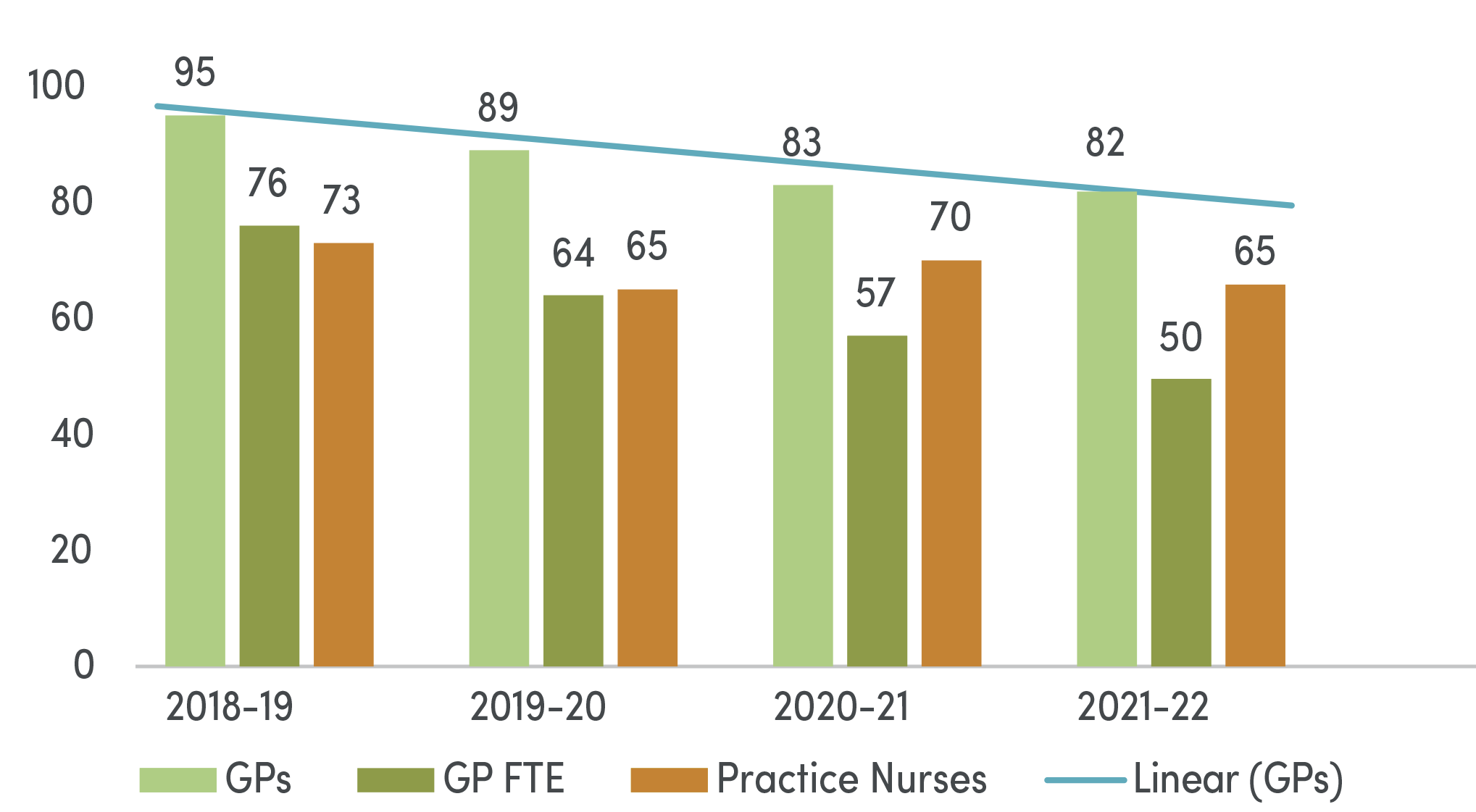
Workforce Challenges
A key challenge for practices across Western Queensland continues to be the decline in GP and Nursing hours available to support the work required to ensure patients have access to proactive, planned and structured care.
Total GPs and Practice Nurse Professionals in General Practice Networks trending year on year:
Telehealth & Digital Health
WQPHN is engaging with all levels of Government and sector stakeholders to improve and accelerate the uptake of telehealth and digital health services in our region, ensuring the needs of remote Australians are considered when policy decisions are made.
Nearly 23 per cent of homes in Western Queensland have no access to the internet - investing in the digital infrastructure to support access to telehealth, online supports, and community, aged care and disability services is a priority.
In 2021-22, 100% of healthcare organisations were provided support to transition from NASH SHA-1 to SHA-2 certificates, allowing them to continue to access digital health platforms and tools, including My Health Record.
Purposeful engagement with the primary health care workforce on digital health news, updates, priorities and opportunities through The Monthly Megabyte, and our Digital Health and Integration newsletter.
We also maintain the Digital Health Help Desk, providing expert advice remotely and in person on key topics and programs such as My Health Record, Secure Messaging, Electronic Prescribing, Telehealth, and the Adaptors to Web Services Program.This year we began work to improve access to Telehealth and After-Hours healthcare for people living in Residential Aged Care Facilities with a goal to increase access to the right care in the right place at the right time and reduce potentially preventable hospitalisations.
In 2021-22 there was 9,915 occasions of service via Telehealth.
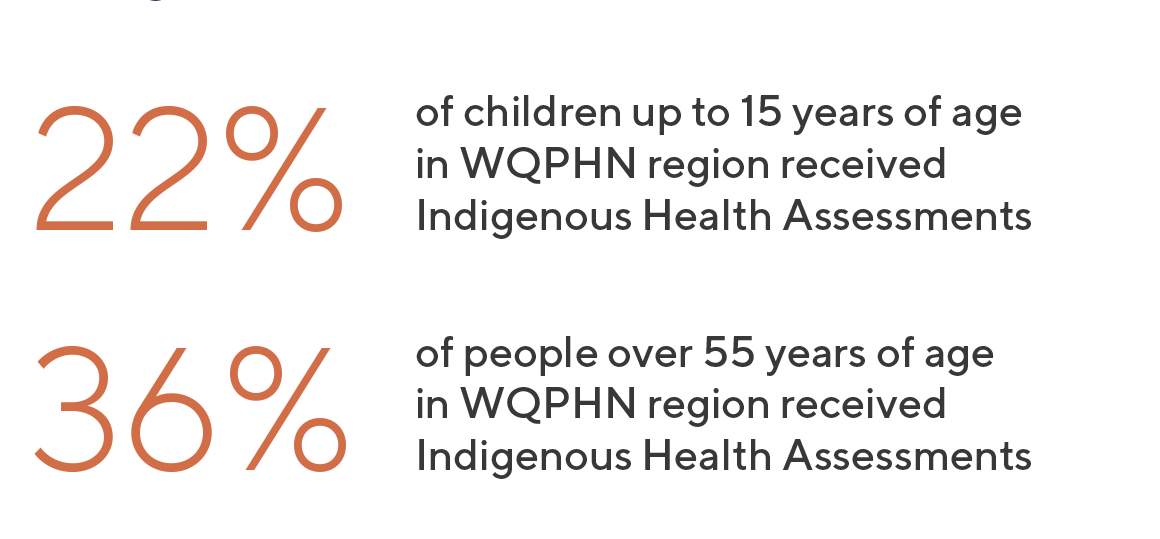
Strategy 3: Closing the Gap
Supporting authentic collaboration and partnership with Western Queensland’s Aboriginal and Islander Community Controlled Health Services (AICCHS) under the Nukal Murra Alliance to strengthen engagement, cultural safety and primary care capacity.WQPHN and Nukal Murra Alliance (NMA) members are working towards lifting the capacity of the primary health care system to increase access to First Nations Health Assessments across the Western Queensland region.
Nukal Murra Health Support Services aim to improve outcomes for Aboriginal and Torres Strait Islander people accessing culturally appropriate mainstream services and care. The goal of the Alliance is to work collaboratively with other funded agencies to support the re-direction of funds to Indigenous Health programs.
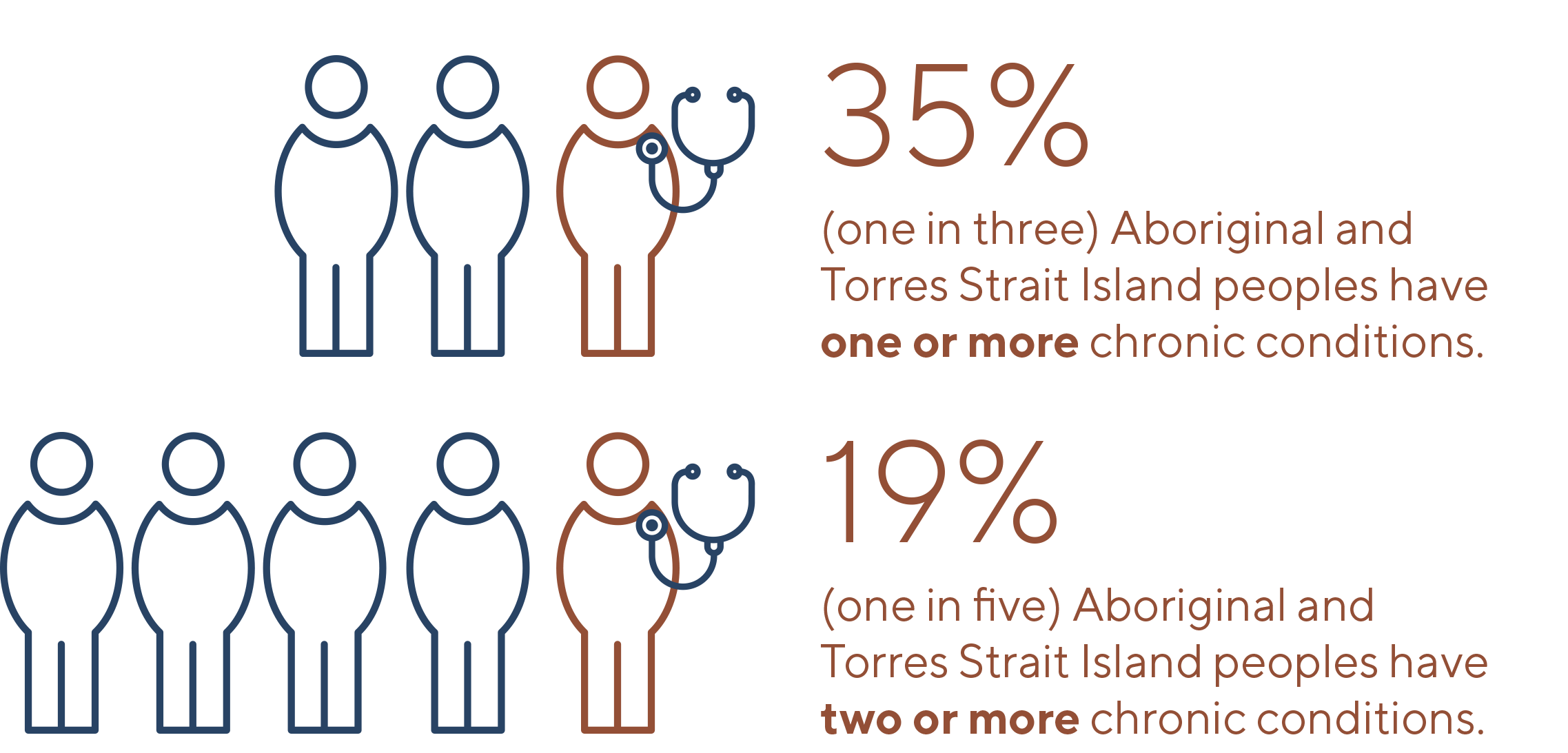
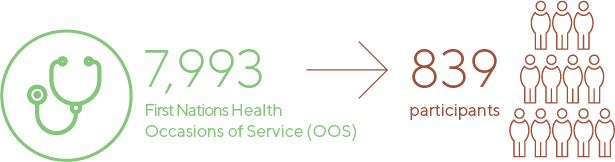
Nukal Murra Alliance provided:

Social and Emotional Wellbeing (SEWB)
WQPHN recruited a full-time Social and Emotional Wellbeing (SEWB) Regional Coordinator to undertake and build capacity of services within the Nukal Murra Alliance (NMA) member organisations. The core functions include enhancing existing commissioned mental health services, and the promotional supports associated with mental health responses for our First Nations people.
The SEWB Mental Health Training and Development Program was provided to two member services by an Outreach Private Consultant Service “Wakai Waian Healing” and Founder- Mr Edward Mosby (Senior Psychologist). The Service provides support with the direct delivery of individual and group therapeutic services, supporting local SEWB Workers and their co-workers with professional development opportunities through mentoring/supervision, and providing direct support and guidance to enhance community and service collaboration and capacity building efforts.
Mornington Island Health Council
Mel Riordan, Rural Health Consulting
When the Mornington Island Health Council developed the inaugural Mornington Island Health Strategy 2019-2024, in partnership with Gidgee Healing, Western Queensland Primary Health Network (WQPHN), North West Remote Health and the North West Hospital and Health Service, the primary goal was to ensure a planned and collaborative approach to improve the health and wellbeing of our community. Since its development, the Strategy has provided a roadmap for government agencies, service providers and other stakeholders to understand the key priority areas for the Mornington Island community.
A soon as it was developed, we realised that we needed to be able to monitor how we were going in achieving the objectives contained within the Strategy. We also wanted to be able to draw on an evidence base and really understand whether the health of our community was improving, staying or same, or perhaps even worsening? It was also paramount that the information was able to be translated in a way that means something to the community. While obtaining reliable health data can be difficult for a community of our size and level of remoteness, WQPHN has worked closely with the Mornington Island Health Council and other partners to identify a data set to enable us to achieve our goals. We have phased our approach, starting with population data, practice data and hospital data that was more readily available. We are in the process of building upon this data set and expanding the information we have available to include other important priority areas, such as early childhood development, mental health and social and emotional wellbeing indicators. Over time, the Data Dashboard will also enhance the capacity of the health service system to identify gaps in service delivery, or similarly, to identify specific areas that may need additional focus.
First Nations Workforce
The WQPHN, alongside our MOU partners, RFDS Qld, CheckUp and Health Workforce Queensland have joined forces with the Nukal Murra Alliance Member organisations to progress a Western Queensland Rural and Remote Aboriginal and Torres Strait Islander workforce strategy for the region.
The Nukal Murra Alliance Members represent the four Aboriginal and Torres Strait Islander Community Controlled Health Services across the West and are the primary employers of the First Nations people across the footprint.
The MOU partners have engaged Petraichor Partners to assist with development of both the strategy and implementation plan to ensure that we put our ideas into firm actions, resulting in growing our own local Aboriginal and Torres Strait Islander health workforce via consultation with key stakeholders.
All partners agreed a sustainable health workforce in rural and remote Queensland hinges on how well they engage with the local community and develop the capacity of local people to undertake roles in health. This not only provides a level of cultural sensitivity for the consumer and the service that’s being delivered, but it also provides opportunities for building careers in health.
“They provide the vital linkages to communities and can ensure that what we build is achievable and realistic, and is geographically, culturally and financially appropriate for the region.”
Diabetes and Prevention Programs
WQPHN commissioned Gidgee Healing to employ a full-time Diabetes Aboriginal Health Worker in November 2021 to coordinate culturally appropriate diabetes education, with an aim to promote and support diabetes management and selfcare, to enhance quality of life and reduce the risks of diabetes-related complications amongst Aboriginal and Torres Strait Islander communities. Many stakeholders have been involved in supporting this exciting new role, including Diabetes Queensland and the First Nations Health Unit. The Western Queensland (WQ) Visiting Credentialed Diabetes Educators (VCDEP) are also collaborating to plan and triage care for people with diabetes in the area, by developing tailored culturally appropriate group education workshops to further support this diabetes care. WQ VCDEP continues to provide diabetes health care professional education to general practices within the WQ region. The program is expanding, and group education has been facilitated in Mount Isa, Charleville and Roma. In late 2021, WQPHN signed on to a three-year contract with My Health For Life, and we introduced the Patient Activation Measure (PAM) in general practices. The Move It North Queensland (NQ) program has expanded to more towns, with virtual delivery methods and capacity building initiatives also being developed for hard to reach individuals and communities.
The Western Queensland (WQ) Visiting Credentialed Diabetes Educators Program (VCDEP) collaboratives to plan and triage care for people with diabetes in the area, to optimise health outcomes to support self- management and care to enhance quality of life and reduce the risks of diabetes-related complications. WQ VCDEP continues to provide diabetes healthcare professional education to general practices within the WQ region as well as developing tailored culturally appropriate group education workshops to further support diabetes care within the community. The program is expanding, with group education being facilitated in Mount Isa, Charleville and Roma. WQPHN commissioned Gidgee Healing to employ a full-time Diabetes Aboriginal Health Worker in November 2021. The program coordinates culturally appropriate diabetes self-management amongst Aboriginal and Torres Strait Islander communities. Many stakeholders have been involved in supporting this exciting new role, including Diabetes Queensland and the First Nations Health Unit.
To further promote prevention activities and programs in WQ, in late 2021, WQPHN signed on to a three-year contract with My Health For Life, and we introduced the Patient Activation Measure (PAM) in general practices. The Move It North Queensland (NQ) program has expanded to more towns, with virtual delivery methods and capacity building initiatives also being developed for hard to reach individuals and communities.
.
Our Stories
Nukal Murra Virtual Home Monitoring
Chronic diseases are long-lasting, and while most are preventable and treatable, they cause approximately 64% of the disease burden among Aboriginal and Torres Strait Islander peoples and approximately 80% of the mortality gap. Virtual Remote Monitoring (VRM) is a digital tool for better management of chronic conditions. Goondir Aboriginal and Torres Strait Islanders Corporations for Health Services (Goondir Health Services) have launched a VRM program.
WQPHN are committed to funding an expansion of the program within the Nukal Murra Alliance, which brings together the WQPHN and the Aboriginal and Torres Strait Islander Community Controlled Health Services (AICCHO) in a regionally focused, culturally informed partnership to improve the health, social and emotional wellbeing of our communities. Goondir Health Services patients are provided with a Bluetooth enabled monitoring device kit. Daily observations from the devices are recorded and transmitted into a portal which is accessed by an assigned clinician. The kit includes a blood pressure monitor, blood glucose monitor, pulse oximeter, weight scale and tablet.
In the program's first year there was 86% of all respondents rated the usability of the equipment as excellent and 58% of clients completed all their vital sign monitoring tasks. There were clinically significant reductions in measured outcomes and evidence of reduced hospitalisations.
Ed Mosby reflects on SEWB Services in North West Qld
“For Wakai Waian Healing (WWH), having the opportunity to partner with WQPHN and Gidgee Healing to deliver Social and Emotional Wellbeing (SEWB) services across Mount Isa and Mornington Island has been a true privilege. Working alongside their frontline SEWB staff and meeting with the organisations management has provided a valuable perspective on the challenges and opportunities that exist in this region when supporting the healing journeys of Aboriginal and Torres Strait Islander peoples.
There is without doubt an ongoing need for SEWB services across the spectrum of need from mild to severe and complex. Our initial observations suggest that one of the most significant challenges relates to establishing a well, competent, qualified, and sustainable workforce. However, facing this challenge head on is possible as there are many strengths that come form building a connection between a workforce and the community from which they more often than not come from. Investment into this workforce through ongoing professional supervision, mentoring, professional development and selfcare initiatives gives rise to opportunities to build the connection between services providers and communities.
It is in this connection that opportunities for healing exist by promoting such principles of empowerment and autonomy and finding a space for both cultural and clinical safety. Promoting a workforce focus within the partnership between WWH and Gidgee Healing is already producing a change in consumer engagement and the capacity of Gidgee Healing SEWB staff”.
Videos:
Strategy 4: Chronic Disease
Improve management and prevention of chronic disease through planned proactive approaches within the WQ Health Care Home model of care, enhancing coordination, patient self-management and independence.After Hours Care for Residential Aged Care Facilities (RACF)
Digital Health in RACFs
The goal for digital health in RACFs is to have the appropriate virtual consultation facilities and technology for residents to access clinically appropriate telehealth care. RACFs can also utilise funding to address internet connectivity, and external support for installation, testing and training, beyond what can be offered by WQPHNs Digital Health Help Desk.
Aged Care facility residents can experience rapid health deterioration during the after-hours period, but immediate transfer to hospital is not always clinically necessary. We will work with our RACF partners to develop and implement after-hours action plans, and while still in a period of co-design at the time of writing, are looking into telehealth emergency services. To ensure continuity of care, uptake and meaningful use of My Health Record will also be a priority.
The WQPHN has funded 5 private RAC in the region to purchase equipment and provide training to enhance their capacity with virtual consultations after hours.
Residents who in the past have been forced to travel several hours to see their GP, now have the choice to see their GP via telehealth, supported by their nurse, in the comfort of their home.
Aged and Disability Care Consultation Forums
In May to June 2022, WQPHN staff and key peak bodies travelled to a number of Western Queensland communities to facilitate Community Consultation Forums for both disability and aged care services in Mount Isa (NW), Charleville (SW) and Barcaldine (CW). These Forums provided an opportunity to hear first-hand about what it is like to access disability and aged care services in the region.
Representatives from the National Disability Insurance Agency (NDIA), Council on the Ageing (COTA) Queensland and the National Disability Services (NDS) participated and were available to give current updates and advice on services available through their agencies. Localised issues around ageing and disabilities in rural communities was evident, with a strong turnout at the three forums.
Thin markets, access to transportation and the costs associated with providing services an underlying theme at all three forums.
Healthy Ageing Programs
Healthy Ageing in WQPHN continued to take a proactive approach to ageing and empower our older community members to be more informed and aware of their health, and to seek ways to live their lives with as much independence and value as they need. To meet these needs aged care funding has focused on connection and providing information for the participants.
Visits were conducted to all commissioned service providers and communities receiving services. These visits allowed the WQPHN to better understand the current and future needs of our communities.
More than 20,000 occasions of service were completed and 170 individuals received services.
In 2022 initiatives such as after-hours and enhanced telehealth support, and the Care Finders program in Residential Aged Care Facilities will improve the outcomes for people seeking aged care services.
HealthPathways
Western Queensland (WQ) HealthPathways is an online resource for all health professionals across WQ. It outlines local clinical and referral information to assist health professionals in providing evidence-based care and make the best use of available services and resources.

Throughout 2021-22, pathways have been released in the child health, respiratory, mental health and substance use specialties. Ongoing work for updating of information for COVID-19 management has been important, and the collaboration between all Queensland regions has allowed sharing of pathways that contain information applicable to the whole state.
Pathways are developed through a systematic process with involvement of local GPs, subject matter experts and health providers. During 2021-22, we welcomed two new GP Clinical Editors, Dr Erica West and Dr Tiffany Cover to the team and celebrated the release of 200 pages since inception.
As we progress into 2022-23, we look forward to continuing work in mental health, as well as localising orthopaedic, dementia, aged care and endocrine pathways.

WQ HealthPathways GP Clinical Editors: Dr Tiffany Cover, Dr Erica West, Dr Karen Benn, Dr Anthony Vogelpoel
WQ HealthPathways Celebrates 200 pathways
Move It NQ
The Move It NQ program was developed in collaboration with the North Queensland Sports Foundation, Northern Queensland PHN, Western Queensland PHN, and Local Government Councils to support healthier and active lifestyles through the delivery of free, place-based sporting and fitness activities for their communities.
Activities are selected that suit a targeted demographic, such as young people, women, or the elderly in any group or region a Council is seeking to assist.
Local Councils including Boulia Shire Council, Carpentaria Shire Council, Cloncurry Shire Council, McKinlay Shire Council, Mornington Shire Council, Mount Isa City Council and Winton Shire Council have embraced the initiative and assisted in providing venues, facilitators, equipment and marketing.
Health benefits of the Move It NQ project include:- Promoting physical activity and lifelong healthy behaviours;
- Encouraging mental and physical health and wellbeing through partnerships with local sport, recreation and health organisations;
- Supporting healthy bones and muscles, heart and lung health and reducing the risk of chronic disease;
- Supporting local councils and organisations in strategic planning and promotion of physical activity initiatives.
The program was extended for hard to reach groups to join in virtually during the 2021-22 financial year, and is now operating or being introduced in additional local government authorities across Western Queensland.
This coordinated approach across Western Queensland is having a positive impact on communities and has been embraced by community members. Click here to read feedback.
For more information visit Move It NQ here
Our Stories..
Aged Care - Barcaldine 60 and Better Program
The Barcaldine 60 & Better program, supported by the WQPHN recently hosted the Barcaldine and District Seniors’ Games in October, one of 23 similar programs across Queensland.
COVID-19 restrictions led to cancellations in previous years but was welcomed back in 2021.
60 & Better Programs are healthy ageing programs designed to encourage people to maintain their interests and participate in all aspects of life through active physical, social and mental interaction.The event was well-attended by the local community, who enjoyed a morning of healthy activities and games , while having access to Wellness and Healthy Living Information.
The local Qld Police Service even joined in the fun!
Participants were provided with a questionnaire to stimulate positive thinking to encourage control of their own health and to seek strategies to enhance their well-being and health literacy.
This and similar programs are not restricted to those over 60 years of age. All people over 50 years are eligible to participate.



Credentialed Diabetes Educators (CDEs) making a difference in community...
A lady with type 2 diabetes recently saw a diabetes educator who spent 90 minutes with her explaining her condition, how her medications work and how high blood glucose levels can impact overall health. This lady was supported to start taking her medication and monitor her diabetes.
One month later the patient came back for a review with the diabetes educator and said, "I wish I was referred to you ten years ago!"
Her fasting blood glucose levels are now in target, she is seeing an exercise physiologist, a podiatrist and an optometrist.
Her mental health is fantastic and she now takes medication because she understands how it works and benefits her overall health, mind, body and soul.
The diabetes educator encouraged this lady to spread the word and help other people in her community who are finding self-managing diabetes challenging to get a referral to a diabetes educator.
Strategy 5: Child & Family Health
Support clinically integrated and culturally safe care across the first 3,000 days of life and improve coordination of services supporting health and wellbeing of children and their families.Healthy Outback Kids focuses on the first 3,000 days of life and pre-natal milestones for Mums.
The program centers around the introduction of regular child health visits and scheduled health checks around critical development milestones and was established in collaboration with the Central Western Aboriginal and Torres Strait Islander Community Health (CWAATSICH), Cunnamulla Aboriginal Corporation for Health (CACH) and the South West Hospital and Health Service (SWHHS).
- All children are enrolled with a general practice;
- Care for each child is scheduled as per the health checks in the Healthy Outback Kids Program;
- Care is delivered by a multidisciplinary team including a General Practitioner, Registered Child Health Nurse, Aboriginal Health Practitioner and Aboriginal Community Workers;
- Service providers share information to ensure all families are offered care program outcomes.

Big Buddy Program

Goondir Health Services continues to deliver The Big Buddy Program on the founded aims to address the four key objectives of:
- Social inclusion
- Mentorship
- Promoting Life Skills
- Education
Goondir’s St George Wellbeing Centre provides the fit for all staff and participants to engage and interact with each other in a number of various activities and well being programs. Stakeholders and other service providers are also encouraged to utilise the Centre teaching young children and youth about product development, ideation and innovation using a fun and interactive activities.
Some highlights over the past 12 months has been the:
- Engagement of “Country University” providing the Big Buddy participants with an opportunity promoting further education and career options and how utilise the facility to further their education experience.
- Through the partnership with “Australian Defence Force (ADF)” recruitment and promotional drive in St George with a number of Big Buddy participants actively participating in a number activities and information sessions on offer within the ADF.
- Health and Wellbeing Queensland providing promotional days and sessions on the importance of staying healthy, eating healthy, promoting exercise, physical activity and fitness.
- Traditional games continue to build self esteem and confidence across all program areas within the local community and encourages all participants the opportunity to build strong networks within the Big Buddy Program.
Goondir Health Services staff are looking forward to the next year with many more innovative activities and programs to enhance the local community.
BUSH Kids
BUSHkids is a not-for-profit organisation which has been supporting the health and wellbeing of children and families with children aged to 13 years in Queensland’s regional, rural and remote communities for over 80 years.
They provide free preventative and early intervention allied healthcare (directly and in collaboration with government & non-government organisations) to children and families who are unable to access services locally due to unavailability or affordability issues.

The BUSHkids team have prioritised support for the holistic development of children transitioning and working from early childhood to Prep in 2023 throughout the WQPHN funded areas. The team continues to build the capacity of Early Years staff to enhance learning opportunities through play, by designing/using activities that support a child’s play as well as their development in line with needs identified through observations in the learning environment.
BUSHkids have been able to build on the work delivered in 2021, by offering ongoing support to the children who previously attended the Mums and Bubs group. Families and their children who are now attending kindergarten have engaged through telehealth support either at home or through the kindy with the support of Hannah the centre co-ordinator.
Working well over the past 12 months:
- Good engagement strategies when working with children and educators;
- Clinicians (OT and Speech) have been able to identify children requiring support once screened with consent gained;
- Feedback from families provided noticing improvements with their children and happy with their child’s development;
- Good foundation of trust and relationships built with staff and educators across all communities;
- Staff and families are receptive to sharing of information from clinicians.
Thuaaka team in Mornington Island
Thuaaka (pronounced ‘thu-ga-ga’) is the name of a small bird that inhabits Mornington Island. In our local Lardil language, thuaaka means ‘happy families bird’. Often encountered in family groups, the thuaaka is a very happy and social bird. Given the importance of addressing the health and wellbeing of our children and young people within a family-centred context, we have adopted the ‘happy families bird’ as a symbol of our broader vision.
The Thuaaka team is a locally-based health and family support workforce established by the Mornington Island Health Council, with support from the WQPHN. The goal is to support the accessibility of health services by children and their families on Mornington Island, to support the achievement of optimal health, development and wellbeing.
The Mornington Health Council believes that the health of our children and young people is intrinsically linked to the health of their family and their home environment, for this reason the Thuaaka team works to ensure child and family health services are responsive and adopt a holistic, family-centred approach, drawing on the strengths of local Aboriginal and Torres Strait Islander cultural knowledge and practices.

The Thuaaka team continues to work with families and other stakeholders within Mornington Island to:
- Actively encourage universal screening and assessment to help families identify and manage health issues earlier;
- Provide Care coordination and case management for vulnerable children and their families;
- Enhance access and engagement with primary health care services; and improve access to other secondary services including education, housing, employment, family violence prevention, and other support services.
How this is done by the team?- Embed cultural competence throughout all aspects of our work which will lead to more effective health service delivery and better health outcomes for children, young people and their families;
- Support service providers and families to build trusting relationships;
- Improve access, attendance and engagement between community and health and social services;
- Increase access to home-visiting and community-based care;
- Improve continuity of care for children, young people and their families;
- Work with services to improve the effectiveness of health and social services.
Indigenous Health Assessments 2021-22
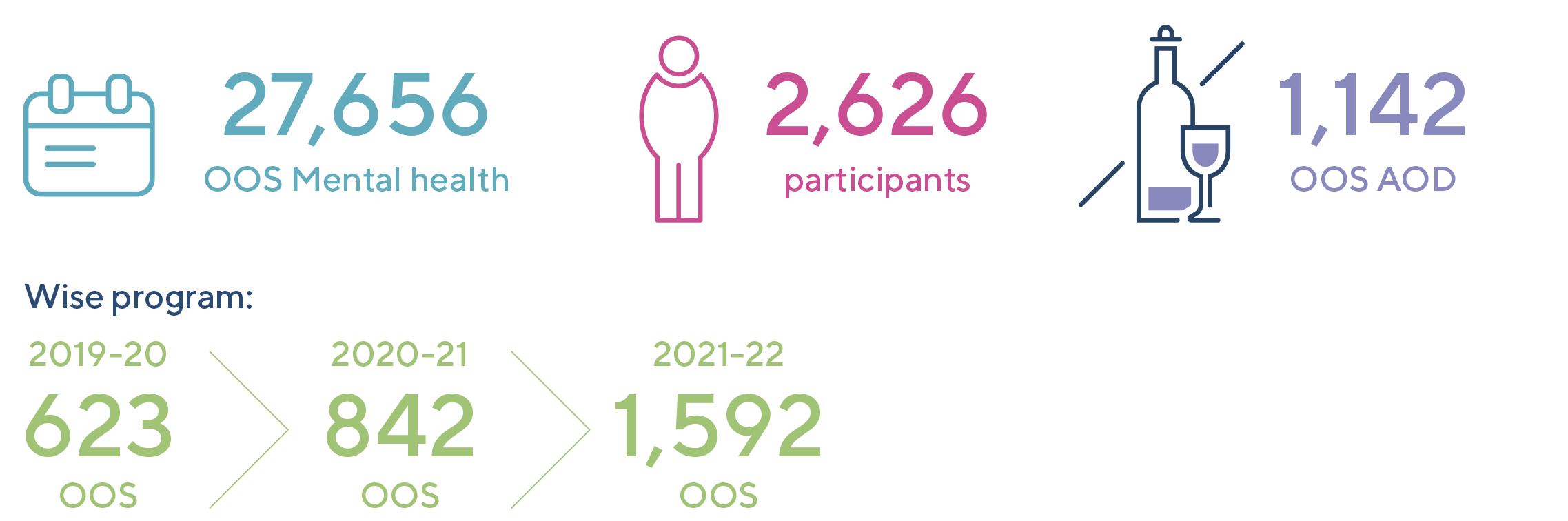
Strategy 6: Mental Health, Wellbeing
Implement a strengths-based approach for those living with Mental Health or Alcohol & Drug issues and enable stepped care with a recovery focus, better coordination and integration across care domains.The MHSPAOD Plan has been completed and is currently being socialised with key mental health consortia partners as we co-commission and collaboration towards Pave Our Way to 2025. This includes ongoing consultation opportunities for key interested parties in each community across the Western Queensland PHN. The Plan is an example of listening to the voices in communities to respond to localised needs, as we develop innovative responses with our partners to address the unique issues relating to mental health, suicide, and alcohol and drugs across the region.
The reinvigoration of this planning process ensures the currency of the ongoing planning of key services and supports in a coordinated and integrated way, maximising existing strengths, resources and infrastructure, and highlighting the diverse needs across all areas serviced by the WQPHN.
The plan also highlights the very unique issues that Western Queensland communities face to inform broader policy responses, as the WQPHN and their partners prioritise areas for service system development and reform to meet the requirements of individuals, families and communities.

AOD Our Way
Discussions in 2020/21 helped shape the Western Queensland 5-Year plan to improve mental health, suicide prevention and alcohol and other drug, and highlighted the need for improved and targeted AOD services in Western Queensland.
The Queensland Aboriginal and Islander Health Council (QAIHC) was commissioned to provide a greater number of locations with access to its suite of contextualised alcohol and other drug (AOD) resources to respond to community and workforce needs regarding harmful levels of substance use.
The initial plan was to provide QAIHC’s AOD training package via face-to-face delivery in a range of Western Queensland communities. However, with increasing infection numbers and COVID restrictions in late 2022 and early 2023, a growing number of small Western Queenslanders expressed concerns about QAIHC’s trainers visiting their remote towns.
With an agreed change to the plan, some of the WQPHN funds enabled QAIHC to partner with Insight to develop e-learning modules and migrate content online – with "Eyez on Ice" now hosted at the Insight website, it provides an online culturally safe resource package designed to assist health professionals and families to support people impacted by problematic substance use, particularly crystal methamphetamine (ice) https://insight.qld.edu.au/toolkits/eyez-on-ice/detail
The development and launch of the Eyez on Ice e-learning modules has helped to widen the reach of this training and the associated resources in remote areas, and also offers greater training flexibility and more platform choice. QAIHC has more recently also delivered face-to-face training in Mount Isa, with key partners such as child and young person’s services staff also included.
headspace
This year has been a productive and exciting time across both headspaces commissioned by the WQPHN - headspace Roma and headspace Mount Isa. headspace centres are funded to deliver services to young people 12-25, who are requiring a range of supports across several areas – including mental health, vocational education, sexual health, alcohol and other drug use.
Mount Isa headspace centre has been at the forefront of engagement of the headspace Early Careers program, ensuring practitioners who are in the early phase of their career have access to quality learning, supervision and support in regional and remote headspace sites. This program ensures access to clinical staff into the future as part of a workforce development and retention strategy for headspaces in remote areas.
headspace Mount Isa was also selected to implement the MOST program – Moderated Online Social Therapy – digital therapy support for young people going through challenging times who may need help with issues such as mental health, employment, study and training, friendship/peer support and family relationships. Whilst delivering face to face modalities, headspace Mount Isa uses blended approaches to engage young people, including one on one therapeutic support, group work and community engagement opportunities, such as local schools in the area, as well as digital health options as required. Mt Isa continues to demonstrate exceptional levels of community engagement and collaborations, and participation by young people in the design and delivery of services.
Roma headspace centre has passed their first year of service anniversary, with a visit by headspace National marking this occasion, and a visit by the WQPHN to celebrate the first birthday with young people in Roma and staff from the Centre. headspace Roma have exceeded headspace National headspace’s expectations in the number of services delivered to young people in the region, evidencing strong engagement and partnerships with the local community, and youth participation, as well as a passion for delivering the much needed services to young people in Roma.
Both headspace centres have demonstrated a significant increase in Occasions of Service and number of service participants across over three years. The difficulties presented by COVID-19 which have impacted on staffing and at times business continuity management, in conjunction with the pressing issues that increasingly impact on young peoples’ mental health, reflects the ongoing need for headspace services in both regions, and funded enhancement to outreach to outlying areas, as well as building capacity to respond to moderate to severe youth mental health issues.
headpace Occasions of Service over time:

QNADA project
Supporting client AOD support in Primary/General Practice settings
Recognising both the disproportionate harm of alcohol and substance use in the region and the key role that place-based general primary health services play in supporting Western Queenslanders to stay well, the WQPHN partnered in 2021/22 with Queensland’s Alcohol and other Drug peak body, QNADA (Queensland Network of Alcohol and Other Drug Agencies).
The intention of the ‘QNADA Project’ is to gradually grow primary health capacity and workforce confidence to engage with people experiencing concerns related to alcohol and other drug (AOD) use. The project builds on the previous AOD-focused capacity building provided by WQPHN (ASSIST and Insight AOD Starter Pack ) and the RACGP/ACRRM AOD trainings rolled out and promoted over the last couple of years.
The QNADA Project has supported primary health services and ACCHOs through the delivery, or continued planned provision, of activities including:
- offering tailored onsite AOD-learning opportunities for primary health agency/clinic staff;
- training in key evidence-based AOD assessment tools;
- AOD development coaching and advice for individual primary health staff;
- Formation and convening of sub-regional AOD networks strengthening the links and referral between generalist and AOD specialist health services.
Commonwealth Psychosocial Support (NPSM / CPS)
WQPHN continues with innovative community focused commissioning under the Psychosocial Support Program.
CPS Brokerage program focused on building wrap around support, continues to change lives of community members with psychosocial disabilities through purchased activities of recovery, independence, and social inclusion. In the 2021-22 financial year, CatholicCare and CentacareNQ continued as commissioned providers with 56 participants received and benefitted from CPS Brokerage Program-funded activities.
NDIS re-testing fund – RHealth was funded in 2021-22 financial period with allied health/psychological assessment assistance regarding NDIS applications. Clientele for this program include current CPS participants and community members with lived experience with psychosocial disabilities that have been ineligible for assistance through the NDIS. 15 clients benefited from this program in 21-22 financial period.
Community Services Facilitators program – Through community-based Facilitators based throughout the WQPHN region, community members including those with psychosocial disabilities have had access to local service navigation assistance to ensure clear and direct pathways to service needs. The aim of the program is to impower local communities to better navigate services and make better informed decisions around their health needs and wellbeing journeys. 249 community members engaged with the Community Services Facilitators with 102 people referred on to additional services.
Wellbeing in Schools Early Intervention (WiSE) Program
The WiSE headspace telehealth e-psychiatry program is a free service launched by WQPHN in collaboration with headspace National Youth Foundation. The program was developed to ensure young people living in rural, regional and remote areas can access a psychiatrist via online consultations in a timely manner, reducing barriers such as the expense associated with access to a highly qualified clinical workforce specialising in young peoples’ mental health, and support to families and carers.
The WiSE service also supports the WQPHN region by providing secondary consultations to professionals who may require upskilling or advice, including GP’s who are treating young people with high needs and more complex presentations. This program has been successfully utilised both through young people accessing headspace, and through the secondary pathway, supporting enhanced clinical outcomes in the youth mental health area.
Telehealth consultations in delivering primary health care services including mental health initiatives increased by 7,976 occasions of service from the 2020-21 financial year to 27,656 occasions of service. 33% of consultations in primary health care were delivered by telehealth in the 2021-2022 financial year.
Our Stories
headspace Roma first birthday celebrations 4 May 2022
headspace Roma celebrated their first birthday on Wednesday May 4, 2022, with local crew and staff enjoying the celebrations, which included a great BBQ, cake, art workshops, games and a chill out zone.
Deb Spanner, WQPHN's Primary Mental Health Coordinator, joined the festivities and spoke with headspace Roma manager Julianne Everson, who proudly reflected on this celebration.
“I can’t believe it’s already a year! It’s been such a pleasure being involved in the set-up of headspace in Roma and seeing the difference it makes not only to the young people involved but their families and friends in the community,” Julianne said.

headspace Roma is a FREE and confidential service that helps young people in the Maranoa Region aged 12-25 with their mental health and well-being, including physical health, alcohol and other drug services, as well as assistance with employment, education and training pathways.
There are currently 110 headspace centres across Australia.website headspace Roma: Roma (headspace.org.au)
Facebook: headspace Roma | FacebookPrimary Health Care Capacity Building Project - Alcohol and Other Drugs
Strategy 7: Good Governance
Provide accountable quality assured corporate, program and clinical governance to support a responsive efficient organisation, focused on improving patient and population outcomes.Corporate, Program and Clinical Governance
There were six Board meetings held across the 2021-22 Financial Year.
Three were held via Zoom, one in Longreach and two in Brisbane.
Clinical Chapter Chairs
Regional Clinical Chapter Meetings have been held over 2021-22 with great attendance and very positive discussions and ideas. These Clinical Chapters are a valuable resource for Commissioned Service Providers across the respective regions and also a network that WQPHN staff members can connect with to share news or discuss emerging issues.
The Chapters are the only multi-disciplinary networks in the region and are represented by the region's Hospital and Health Services (HHS), Allied Health, Mental Health, AOD, Nukal Murra, Aged Care, GPs and pharmacy.
This year has seen the handing of the flame to new leaders for each region – Jean Benham (South West), Cassie French (Central West) and John Cain (North West) who are eager to lead the teams.

"As an Allied Health clinician, consumer and long-term local, my focus as Chair of the South West Clinical Chapter is to support engagement to allow family, friends, work peers and staff contribute to community wellness, with an emphasis on developing equitable access to Allied Health services in health care. Representatives of the Chapter “dig deep” into how the value of the group can be grown for each organisation in their pursuit of health service for people of South West Queensland.
Clinical Chapters are such a significant opportunity to support each other in improvements towards our shared vision to ensure the viability of high-quality health care, meaning “the right care at the right time and in the right place” - Jean Benham, Vital Health, CEO

"As the Regional Coordinator for Central and Central West Queensland at CheckUP, I am actively involved in stakeholder engagement, contract management and service development across the region.
I am passionate about preventative health and early intervention, and love being involved in work that helps to increase access to health services and creates sustainable outcomes. My role at CheckUP meant I could return to the Central West (where I lived and worked for 5 years) to help contribute to improving health outcomes in these remote areas.
I am a big believer in conversations and working together to make a difference, and the Clinical Chapter meetings are a great way to be involved in this with key stakeholders and community members.
Clinical Chapters are invaluable to facilitating discussion between service providers, with respect and fairness and focusing on priority needs of the region, resulting actions and achievable outcomes for the year." - Cassie French, CheckUP, Regional Coordinator

"As CEO of NWRH, I took on the role of the North West Clinical Chapter Chair to support our communities and each other through the exchange of information, and to ultimately improve the overall health care opportunities for all within Western Queensland.
The Clinical Chapter(s) play an important role in advancing health intelligence and health outcomes for these Western Queensland communities.
Clinical Chapter groups are a tremendous opportunity to continue to build on the great work done to date and to advance the overall health care opportunities in Western Queensland" - John Cain, NWRH, CEO
Primary Health Insights - Outback Insights
WQPHN is participating in a new national technology initiative known as Primary Health Insights, initiated to simplify and standardise governance, systems and processes associated with data storage and analysis.
The Primary Health Insights program (locally rebranded by WQPHN as Outback Insights) will:
- increase PHN analytical and reporting capability
- reduce duplication of effort
- simplify processes
- automate manual data and governance processes
- standardise reports where possible
- reduce IT costs.

A new highly secure lockbox environment has been built within the Primary Health Insights environment, with WQPHN retaining full custodianship of data. The onboarding process involved a comprehensive assessment and audit of WQPHN’s data governance and privacy measures, to ensure the organisation is operating at a suitable maturity level to join Primary Health Insights. WQPHN successfully completed the onboarding audit and our team was commended for the high quality of our policies, procedures and systems in place to maintain data privacy and cyber security.The Outback Insights project aims to improve the use of data to enable WQPHN to meet objectives around improving population health outcomes.
Financial Statements Summary
7.1 - 2021-22 Annual Financial Statements SummaryView financial data via PDF links:
-
Directors' Report & Declarations
-
Financial Report - Statements of Comprehensive Income & Financial Position
-
Auditor's Declarations
Our Stories...
headspace Roma 1st birthday
headspace Roma celebrated their first birthday on Wednesday May 4, 2022, with local crew and staff enjoying the celebrations, which included a great BBQ, cake, art workshops, games and a chill out zone.
Nukal Murra Virtual Home Monitoring
Chronic diseases are long-lasting, and while most are preventable and treatable, they cause approximately 64% of the disease burden among Aboriginal and Torres Strait Islander Peoples and approximately 80% of the mortality gap.
COVID-19 and Aged Care
The steady achievers in 2021/22 have once again been the committed staff working in residential and community aged care.
Telehealth and Digital Health
Nearly 23 per cent of homes in Western Queensland have no access to the internet - we need to invest in the digital infrastructure to support access to telehealth, online supports, and community, aged care and disability services.
Healthy Ageing Aged Care Roadshow
WQPHN collaborated with Mable to visit regional communities throughout Western Queensland to discuss options for community-led aged care services and provide workforce solutions for rural and remote areas.
WiSE Mental Health & Telehealth
WQPHN has commissioned headspace National to provide the Wellbeing in Schools Early Intervention Telepsychiatry program (WiSE).
Credits
The WQPHN website was developed and is maintained by Michael R.G. Hughes of Extremely Geeky.
Disclaimer
While the Australian Government Department of Health has contributed to the funding of this website, the information on this website does not necessarily reflect the views of the Australian Government and is not advice that is provided, or information that is endorsed, by the Australian Government. The Australian Government is not responsible in negligence or otherwise for any injury, loss or damage however arising from the use of or the reliance on the information provided on this website.